Development of the spine
Molecular and cellular tissue interactions, as well as increasing organ complexity, characterize the fundamental features of the embryonic developmental process during axial embryogenesis. Alteration in the molecular and macromolecular process may lead to structural defects involving the spine and spinal cord. Such defects may occur prenatally and/or postnatally and, from the standpoint of basic developmental pathogenesis, can be divided into the following 3 categories:
- Malformation
- Disruption
- Deformation
Malformation
Malformation is a failure of the embryologic differentiation and/or development of a specific anatomic structure, causing it to be absent or improperly formed before the fetal period commences. (An example is the formation of a hemivertebra.) Once it is established anatomically, the defect may continue to affect spinal development adversely throughout the subsequent fetal and postnatal periods. The type of malformation and its severity depend on the stage of the developmental or maturation cycle that is specifically affected.
Disruption
Disruption refers to the destruction of an anatomic feature that formed normally during the embryonic period. This phenomenon, resulting in a structural defect, involves the limbs (amniotic band syndrome) more frequently than the spine, during the fetal stage.
Deformation
Deformation is an alteration in the shape or structure of an individual vertebra or of the entire spine during the fetal and/or postnatal periods, after the involved region's initial, normal differentiation. Infantile scoliosis and adolescent scoliosis are examples of conditions resulting from deformation and are therefore not true congenital forms of scoliosis. Deformations may be divided into those that are intrinsically derived and those that are extrinsically derived.
Intrinsic deformations result from the reduced ability of the fetus or child to move away from normal imposed forces and depend on the integrity of the neuromuscular system to respond effectively. Extrinsic prenatal deformations are the result of reduction in the amount of space in which a developing fetus may move. Such reduction may be either physiologic or pathologic.
Physiologic structural deformation usually is limited and relatively reversible once the constraining influences are removed. In contrast, pathologic structural deformation is a more permanent process.
Late gestational deformations have an excellent prognosis. Approximately 90% of such deformations noted at birth correct spontaneously. The earlier a deformation is recognized, the greater the likelihood of correcting it or at least preventing further deformation (with, for instance, early bracing for idiopathic scoliosis).
Embryogenesis
Gestation has been divided into the embryonic period and the fetal period. The embryonic period is considered to be the time from fertilization to the end of the eighth week of gestation. The remainder of gestation is called the fetal period. By the end of the embryonic period, all of the major organ systems have been established, and the basic body plan is complete. The 5 major stages of embryonic development can be summarized as follows:
- Fertilization - Female and male gametes combine to form a zygote.
- Cleavage - The zygote divides into a ball of smaller cells, each receiving different parts of the maternal cytoplasm.
- Gastrulation - The cells migrate and proliferate to form the 3 primary germ layers, namely, the ectoderm, the mesoderm, and the endoderm.
- Neurulation - The notochord, neural crest, and precursors of the central and peripheral nervous system form.
- Organogenesis - Primary cell types differentiate to generate the organs.
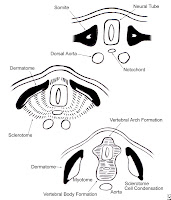
The spine has its embryologic origins in the cell that is induced to migrate out of the somite and toward the notochord and the neural tube . As a mass of sclerotomal cells collects segmentally at the embryonic midline, surrounding the neural tube and the notochord, the sclerodermal cells begin to separate into a cranial portion and a caudal portion.
T
he cranial portion of each sclerotome recombines with the caudal portion of the directly superior sclerotome in a resegmentation process known as metameric shift.After the metameric shift, spinal nerves, which originally left the neural tube to go to the center of the sclerotome, are able to pass between the precartilaginous vertebral bodies to innervate the segmentation myotomes
The atlas and axis form by a mechanism that is different from that of the other vertebral bodies. Part of the first cervical sclerotome plus the cranial portion of the second cervical sclerotome contribute cells, forming the odontoid process and the arch of the atlas.
In the cervical region, the 8 cervical somites generate 7 cervical vertebrae because the cranial portion of the first cervical sclerotome contributes to the formation of the occiput and the caudal portion of the eighth cervical sclerotome contributes to T1. In this way, the 8 cervical spinal nerves become associated with 7 cervical vertebrae The first cervical spinal nerve passes between the base of the skull and the first cervical vertebra. The eighth cervical nerve exits below the seventh cervical vertebra and above the first thoracic vertebra. The remainder of the nerve roots exit below their corresponding vertebral bodies.The intervertebral disks form in the area between the resegmented vertebral bodies after the split of the sclerotomes. The nucleus pulposus originates from cells of the notochord, whereas the annulus fibrosis originates from the sclerotomal cell.
At the same time that the sclerotomes are undergoing a shift to form the vertebral bodies, the heart, kidneys, trachea, and esophagus are differentiating, which means that a noxious influence during this time can affect the adjacent, simultaneously developing organs. Hence, cardiac anomalies often are associated with congenital scoliosis of the thoracic spine, and renal anomalies are often associated with congenital malformation of the lumbar spine. VACTERL syndrome (abnormalities of the vertebrae, anus, cardiovascular tree, trachea, esophagus, renal system, and limb buds) is an extreme example of association of malformation in the embryonic stage.
Genetics
A family history of congenital spinal deformity is rare. Winter and colleagues found that only 13 of 1250 patients had a positive family history of such deformity Studies of twins usually have shown that if 1 twin has an anomaly, the other does not, even if the twins are identical. However, several investigators have described hereditary congenital scoliosis. Most of the patients in those reports had extensive defects of segmentation in association with spondylocostal, costovertebral, or spondylothoracic dysplasia (Jarcho-Levin syndrome). In addition to spinal segmentation defects, segmentation defects often occur in the ribs, leading to the development of a small, stiff thorax and, frequently, to pulmonary compromise. Such defects also may extend into the cervical spine as a Klippel-Feil anomaly.
Article taken from
medscapeCongenital Spinal Deformity
Author: Robert Mervyn Letts, MD, FRCS(C), FACS, Former Chief, Department of Surgery, Division of Pediatric Orthopedics, Children's Hospital of Eastern Ontario, University of Ottawa; Consultant Pediatric Orthopedic Surgeon, Sheikh Khalifa Medical City, UAE
Coauthor(s): Ayman Hussein Jawadi, MBBS, Pediatric Orthopedic Consultant, Department of Surgery, King Fahad National Guard Hospital